LONG COVID
Neuroplastic & Mind-Body Resources
Written and Compiled by Kent Bassett
Note: people with Long Covid often suffer from related illnesses like POTS, ME/CFS, migraines, headaches, fibromyalgia, and irritable bowel syndrome. We have resource pages for each of those as well.
JUMP TO TOPICS
• MOLLY’S STORY WITH LONG COVID
• What is Long Covid (LC)?
👉 New! Harvard BRAIN RETRAINING Study Shows Astonishing ResultS for unlearning LONG COVID
👉 NEW! Watch the Replay of our webinars with two doctors who successfully treat LC patients
👉 New! … TWO Thoughtful Articles about LC that acknowledge brain retraininG
• LC Recovery Stories that Inspire Hope
• Blind Spots in THEORIES that LC Must Be a Structural Disease Process
👉 NEW! NIH RESEARCH: “we are finding little to no abnormalities” in lc patients
Molly’s Story
It was August 2022 when Molly, 34, contracted Covid-19. For over two years she had avoided the infection, but she was finally exposed at a mandatory work event. Molly had been a bit anxious about Covid-19; she had asthma and worried about the virus’s effects, and family members were additionally nervous from what they read in the news about Long Covid. It was a particularly stressful time at work in a relatively new job, and Molly’s symptoms were not worrisome—mostly fatigue and what felt like a bad cold. She was anxious to get back to work and exercise when she started feeling better five days after testing negative.
But a long and extremely grueling workday made her feel the next morning as if she had the worst hangover of her life. Symptoms of extreme fatigue and congestion returned, and Molly also began to experience rapid heart rate, known as POTS. Through conversations with her doctor and reading Reddit forums online, Molly researched Long Covid, and learned about how people were experiencing and treating their symptoms—from fear mongering to support groups, supplement regimens to blood transfusions, and more. Because it hadn’t been three months since she tested positive, the official period considered by medical professionals to indicate Long Covid, Molly wasn’t able to seek treatment from her doctor. But on her own, she continued to research Long Covid online and tried to understand and alleviate her symptoms through various means, including heart-rate monitoring, compression stockings, salt loading, physical therapy specifically for Long Covid, and a 10-day course of Paxlovid; she eventually had her bloodwork done, her heart and lungs checked, and no structural damage was discovered. At month three, Molly was feeling as bad as ever, and growing more frustrated and worried that her symptoms might never lift.
A turning point came in Molly’s research when she discovered a study that showed that blood clots and microclotting—which she noticed was frequently reported in online Long Covid forums as one example of structural damage when others could not be found—can be caused by the sympathetic nervous system ("Historical studies on the physiology of the sympathetic nervous system (SNS) attributed accelerated blood clotting to the components of the fight-flight response."). She also learned that POTS was first recognized as a symptom soldiers suffered from after returning from the traumatic experience of war. “Somehow that just made me realize, like, ‘Oh, I could see how [my] symptoms would be triggered by the nervous system,’” she says. Molly knew that contracting Covid-19 had been a traumatic event for her after a fearful couple of years, and that it happened at a particularly stressful time in her life.
Around this time, she also discovered a podcast that described people’s recoveries from Long Covid using a mind-body approach. She decided to give it a try, and enrolled in two programs: first Dynamic Neural Retraining (DNRS) and then the Lightning Process (a three-day program). She took off from work in order to dedicate herself fully to the programs, which required Zoom meetings, videos, readings, and exercises. The accountability from the facilitator and the group made her feel supported, and soon she was going on long walks and bike rides that wouldn’t have seemed possible just weeks before. Molly felt about 80% better after starting the program, and completely better 8 weeks later. She is now able to exercise, travel, and work without any limitations.
“My experience with recovering from Long Covid made me realize that my brain could create these very real physical symptoms,” she says. Almost immediately, she began to feel better, which gave her confidence and hope. From there, “I was able to recover from all of my injuries.” Today, nine months after she initially contracted Covid-19, she feels back to normal.
“I would encourage people to give this a shot before they try other invasive things,” she says. “I am a very rational person, and I really feel like I did my research around all the other possible options.” When she knew her symptoms were not caused by structural damage, and she realized the powerful links between the mind and the body, she was open to trying a mind-body approach.
“This is a big shift in the way that we think about healing and what we've been taught about how our bodies work and how Covid works. You don't need to be 100% on board. You just need to be open to it. You need to be like, ‘Is this a possibility?’ And like if you feel like it's a possibility, then it's worth trying out. As you start to feel better, you will get more evidence and that evidence will help shift your belief.” Molly’s story is a testament to this shift in belief, and a success story of recovering from Long Covid through a mind-body approach.
What is Long Covid?
Long Covid describes the experience of symptoms that linger long past the standard recovery time for a Covid-19 infection, typically defined as three months after initial infection. Because it is a new, varied, and complex phenomenon, it can be difficult to talk about it. A large number of people suffering from prolonged effects of Covid-19 have structural issues like lung damage, heart damage, or other physical damage. Some who were in intensive care wards experience Post Intensive Care Syndrome (PICS), in which health problems remain after recovery from a critical illness. But a significant portion of people suffering from Long Covid symptoms—such as widespread pain, fatigue, insomnia, and brain fog, symptoms often attributed to a “post-infectious syndrome”—have no identifiable structural issues, and are commonly known as “functional” or “medically unexplained” symptoms (some sufferers of Long Covid even test negative for antibodies). This makes some Long Covid cases fit within the category of “functional syndromes,” which includes fibromyalgia, irritable bowel syndrome, migraine headaches, chronic Lyme disease, and chronic fatigue syndrome (ME/CFS). In these cases, it can be difficult to know how to treat symptoms that have no identifiable origin or easy explanation, but are nevertheless real, despite the lack of structural damage to explain their cause.
This Might Hurt explores the latest neuroscience to explain how many long-term illnesses, while perhaps triggered by an initial infection, can be learned by the nervous system, sometimes leading to disability. Neuroplastic brain retraining (or a mind-body approach) can be very effective for functional somatic disorders. These evidence-based treatments can help by reducing fear and calming the nervous system. In this way, some illnesses can be unlearned and reversed. One brain retraining technique, Emotional Awareness and Expression Therapy (EAET), has been shown to be effective in a randomized trial for patients with fibromyalgia, and was listed as a “best practice” by the Department of Health and Human Services on the strength of the data.
There is a well-known history of stigmatizing patients, especially women and people of color, whose syndromes are not yet clearly understood through biomedical investigation, and this extends to the treatment of Long Covid. Instead of dismissing these people and their real symptoms because of what we don’t fully understand, medical professionals like Dr. Schubiner and physicians at the Psychophysiologic Disorders Association (PPDA) work to understand how a mind-body approach might help patients recover. This Might Hurt illustrates what a step-by-step, evidence-based mind-body treatment looks like for when doctors “can’t find anything wrong.”
While there is currently a raging debate about the cause of Long Covid—whether it is an as-yet unidentified organic structural disease process, a brain-generated mind-body condition, or both—we’re seeing some promising signs that our film is relevant for many Long Covid patients, especially those without identifiable damage. Even for people who do have structural damage, brain retraining may be an effective method for reducing fear, regulating the nervous system, and unlearning symptoms like fatigue and pain. Since the release of This Might Hurt, Dr. Schubiner and his colleagues have reported that patients with Long Covid can indeed recover using the same mind-body healing principles we explore in the film. He is cautiously optimistic that a significant portion of the millions experiencing Long Covid have a neuroplastic, reversible condition. Meanwhile, reputable institutions like the Mayo Clinic are releasing statements saying “The mind and body do work together. And both need to be addressed in treatments for this condition [Long Covid].”
STUDIES, ARTICLES, RESOURCES
A Study at Harvard Shows Remarkable Reductions in Long Covid Symptoms
There are currently no approved medications for treating Long Covid. There are proven brain retraining—mind-body treatments—for pain and fatigue. And now they have been tested for Long Covid and found to be effective, with pain going down 50%, trouble breathing going down 80%, and fatigue going down 44%, brain fog going down 67%.
“At baseline, 13 of 23 participants (57%) indicated that they strongly agreed with the statement that exercise made their symptoms worse. [After mind-body treatment] only 1 (4%) participant strongly agreed.”
Michael Donnino, MD, the lead investigator of the study, is a professor and emergency medicine doctor at Harvard Medical School who takes care of Covid-19 patients in the ICU. His work has been published in NEJM, JAMA, the British Medical Journal. He and his team have recently released results for a brain-retraining treatment for Long Covid patients.
As a pilot study with 23 participants, it was not randomized—the next trial, with a control arm, is in progress.
The study is very promising for LC patients as it shows that they experienced significant reductions in symptoms. This is a nearly identical treatment that you can see in our film, This Might Hurt, and the patients in his study used the same workbook as those in our film: Unlearn Your Pain.
All of the people in the study had organ damage ruled out before they were admitted, and were ineligible if they had been in the ICU with Covid-19. (According to Dr. Donnino, the tests for lung damage are CXRs, CT, and PFTs; for heart damage, ECHO, MRI; for brain damage, CT and MRI; and for kidney damage, chemistry tests.) This exclusion criteria was used because the brain retraining treatment is generally recommended for people who don’t have clear signs of structural damage.
SSS-8 refers to somatic symptoms score, including “gastrointestinal, pain, fatigue, and cardiopulmonary aspects of the general somatic symptom burden” (citation: JAMA article on SSS-8))
Dr. Donnino has posted on Twitter about his findings, where you can follow the conversation.
Free: Watch the Replays of Our Live Seminars with These Practitioners:
> Rebecca Tolin
> Lilia Graue, MD
> Michelle Wiegers
> Rebecca Kennedy, MD
Brain retraining and mind-body treatments for pain, fatigue, POTS, and Long Covid are sometimes criticized for dismissing women’s suffering. These practical discussions, moderated by directors of This Might Hurt Marion Cunningham and Kent Bassett, bring a feminist perspective to this controversial topic, and discuss how these treatments have affected their lives and the lives of their patients and clients.
In the below video, Rebecca Kennedy, MD discusses how she successfully treats Long Covid patients at Kaiser Permanente in Oregon. (Jump to the chapter at minute 54 for LC details.) The earlier part of the conversation with Dr. Kennedy details the whole treatment protocol that was alluded to briefly in the above seminar with Lilia and Michelle.
Are the Default Assumptions about Long Covid in the Media Accurate?
Photo-Illustration by Intelligencer
“Has Long Covid Always Existed?”
Jeff Wise in New York Magazine
Jeff Wise published a thoughtful piece about Long Covid in New York Magazine that traces the tangled history of how advocacy of ME/CFS has resulted in the federal government spending $1.15 billion to research Long Covid as a strictly biomedical disease, rather than looking into psychosocial components of the illness and its potential remedies. So far, that staggering sum, $1.15 billion, has not led to any notable advances in the understanding of Long Covid. Not a single promising treatment was identified or studied.
“The biological theory of long COVID, like that for ME/CFS, still lacks compelling evidence. An NIH study (https://pubmed.ncbi.nlm.nih.gov/35605238/) published this May found that patients who’d tested positive for COVID and met the criteria for long COVID did not show any biomarkers for illness or any trace of residual virus.
Nor did they show evidence of inflammation, immune system activation, or any organ damage. “We’ve not yet been able to identify a single, repeatable, reliable, objective marker,” Bateman, the ME/CFS doctor, acknowledges. How sick a person gets from acute COVID didn’t seem to have any bearing on whether they will later get long COVID, either.
A study conducted this year (https://www.nature.com/articles/d41586-022-01453-0) found that getting vaccinated didn’t much affect a person’s chances of coming down with long COVID, as you’d expect if it was triggered by the virus.”
Access the article by Jeff Wise in New York Magazine:
Wise’s piece unfortunately does not discuss science-backed protocols that have been specifically tailored to address brain-induced physical symptoms, namely Pain Reprocessing Therapy (PRT) or Emotional Awareness and Expression Therapy (EAET).
Wise cites CBT and graded exercise therapies as if they are the go-to psychological therapies for ME/CFS and Long Covid. These are the same therapies that compose the world of “pain management,” which typically does not address root causes of Long Covid and similar illnesses like ME/CFS, fibromyalgia, and Chronic Lyme Disease, though they can be helpful for some. For getting to the root cause of suffering and providing relief, PRT and EAET have better results in randomized controlled trials.
From The New Republic:
“We Might Have Long Covid All Wrong: Some post-Covid symptoms may be produced by the brain. Does that make them any less real?”
By Natalie Shure
Shure’s article argues that psychosocial factors are a significant and misunderstood contributor to some illnesses, likely including many cases of those experiencing Long Covid. It explores how common symptoms such as fatigue, brain fog, and chronic pain have largely eluded modern medicine, and the competing biomedical and biopsychosocial frameworks for understanding them. Unfortunately, the article also fails to mention NIH-approved treatments, like PRT and EAET, that can resolve Long Covid symptoms.
Shure points out that Long Covid is in many cases a functional somatic syndrome—no lung or heart or organ damage is found— and so it is similar to other illnesses like functional neurological syndromes (FND), and may never have a medication that resolves it. Doctors have known about FND since before 1900 and there is still no medication for it. Yet she points to hopeful stories of how people have unlearned their FND symptoms nevertheless, without any biomedical intervention. The whole article is worth a read.
Unfortunately, the article also fails to mention NIH-approved treatments, like PRT and EAET, that can resolve Long Covid symptoms.
“There is unlikely ever to be a penicillin for long Covid or ME/CFS. Indeed, even as we’ve churned out pills and shots that target specific pathogens and render the scourges of yesteryear practically irrelevant, we’ve never gotten very good at treating some of our most common chronic symptoms, such as brain fog, fatigue, and pain. Drugs can zero in on a pathogen, but they aren’t so good at targeting the biopsychosocial factors that shape our well-being.”
An open-letter response to Shure argued that the article included inaccuracies; Shure emphatically disagreed in a response piece on Medium, in which she argues that her article was mischaracterized by the letter, and responds point by point.
Becca Kennedy, MD is interviewed below about how neuroplasticity can be the cause and the cure of Long Covid.
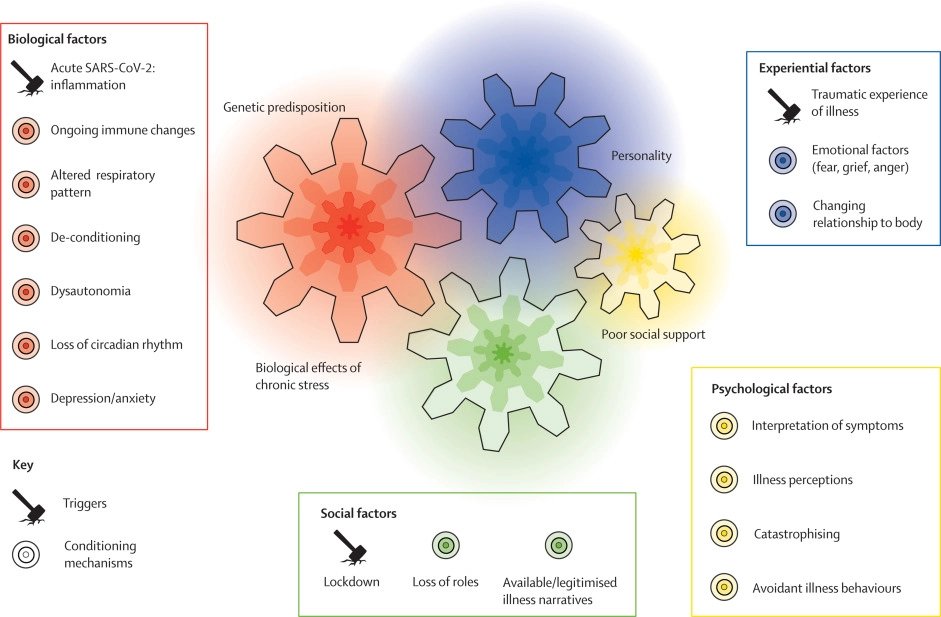
The Emerging Biopsychosocial Model of Long Covid from The Lancet
This commentary in the Lancet, “A new paradigm is needed to explain long COVID,” outlines the importance of not exclusively focusing on the biological, but also incorporating the psychosocial aspects of Long Covid for treatment.
“A new paradigm is needed to explain long COVID…
We suggest it is time to break taboos based on a dualistic understanding of physical versus mental illness and bring in existing knowledge about functional somatic symptoms to provide improved explanations and treatments.”
The authors visualize their proposal for biopsychosocial view of Long Covid this way:
Is Long Covid Neuroplastic?
After an infection has been fought off by the immune system, the nervous system can get stuck in “sustained fight-or-flight mode,” which has neuroplastic feedback loops that can be learned and unlearned.
The New York Times published an opinion piece with a helpful perspective on Long Covid by medical professors at Harvard and Johns Hopkins.
The Truth About Long Covid is Complicated. Better Treatment Isn’t.
They write that “psychosocial strain” of the pandemic lockdowns was a likely contributor to Long Covid.
“We must move beyond a false mind-body dichotomy that stigmatizes physical symptoms that are bound up with mental suffering.”
A study published in JAMA Psychiatry found that psychological distress was predictive of increase risk of developing Covid-19.
“Sustained psychological distress may cause activation of the hypothalamic-pituitary-adrenal axis and subsequent immune dysregulation.”
How are Long Covid Patients Being Dismissed?
Many Long Covid patients are being met with disbelief by their doctors. They are questioned as if they don’t understand their own bodies, or they’re told “it’s stress,” “it’s anxiety,” “it’s all in your head,” simply because no objective evidence of tissue damage was detected. This is a well-known problem of stigmatizing patients, especially women, whose syndromes are not clearly understood—yet—through biomedical investigation.
Our film This Might Hurt explores the latest neuroscience that many long-term illnesses, while perhaps triggered by an initial infection, can be learned and locked in by the nervous system and cause disability. Through reducing fear, calming the nervous system, and doing brain retraining, some illnesses can be unlearned and reversed. We’re seeing some promising signs that our film is relevant for a subtype of LC patients.
Howard Schubiner’s experience with Long Covid patients
Alt-Text: Video of Howard Schubiner discussing Long Covid during a Q&A for This Might Hurt.
Success Stories: Unlearning Long Covid by Retraining the Brain
Below are success stories that are generally based on the brain-retraining protocol you can read more about here.
An Infectious Disease Doctor Develops Long Covid and Tells His Remarkable Story
Dr. Paul Garner is a “medical researcher and clinician who specializes in the biological communication between the body and the brain.” He fell ill for months with Long-Haul Covid Syndrome and wrote extensively about his debilitating symptoms in the British Medical Journal (BMJ). He recovered through neuroplastic retraining and described what helped him in the BMJ and in the Guardian.
“I learnt that our primitive and unconscious defence mechanisms against injury and infection in the brain and other parts of the body sometimes get disturbed, giving false fatigue alarms. A vicious cycle is set up, of dysfunctional autonomic responses being stimulated by our subconscious. These neural tracks become established like tyre tracks in mud. I learnt that I could change the symptoms I was experiencing with my brain, by retraining the bodily reactions with my conscious thoughts, feelings, and behaviour. Over the following weeks, with support, I learnt how to do this. I suddenly believed I would recover completely. ”
And here is a video of him telling his story:
Here’s a young man who successfully used meditation to overcome debilitating fatigue:
“Defogging My Life” Podcast Interview with Fiona about overcoming Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS). This is of course not about Long Covid, however, ME has very similar post-infection symptoms as Long Covid, so there is much in this interview that is also relevant for Long-Haulers.
Collection of Long Covid Success Stories by Sarah Rainwater and friends
“How I Finally Healed When I stopped Believing a Diagnosis of Incurable,” an ME/CFS Recovery story by Rebecca Tolin. She describes how she overcame post-exertional malaise.
Interview with Sarah Rainwater was produced by Rebecca Tolin.
Dan Buglio (a mind-body health advisor/coach) interviews Jake about overcoming Long Covid. (Dan Buglio uses the term TMS, which is a synonym for “brain-induced condition” or “mind-body syndrome.”)
“The one thing that I found so effective is using language in the moment. Like walking, at the time I couldn’t walk for more than five minutes. In my mind I was like ‘Oh god, am I going to crash?” They get you to think about language, for example, just repeat, “I am safe.” And it sounds so small. But when I would crash, I would feel really unsafe. I learned when you’re engaging in those activities, to reinforce “I am safe.... I am safe...” The first time I did this, I could walk for 15 minutes. And I was like “Did that really just happen? Surely not, surely that did not just happen.” I ended up becoming more open-minded to these types of things. [...] It was only when I believed recovery was possible that progress could start.” ”
“Body Politic” is an online group that is organizing around Long Covid and offering community, and they have meditation groups that support people struggling with LC. Some of the members participate in brain retraining programs like DNRS or Gupta Program, or others. Here is a success story from DNRS (we are not affiliated with them, but many people find it helpful).
For some people, changing thoughts and beliefs and reducing fear is sufficient to recover and heal, whereas for others doing emotional processing along the lines you can see in This Might Hurt is a critical step in their recovery.
POTS-specific story
4 min video about one woman’s story with Postural Orthostatic Tachycardia Syndrome (POTS), a symptom that is reported by some people with Long Covid (there’s a lot more you can do besides “think positively,” but addressing thought patterns can be a key part of recovery.)
What are the theories about Long Covid being a structural disease process?
It’s still early in the research process for understanding how the novel coronavirus affects people long-term. Journalist Julia Belluz at Vox summarized the current theories after a conversation she had with Yale immunologist, Akiko Iwasaki, PhD.
The theories are:
(1) there may be reservoirs of virus or virus fragments that are still causing damage to particular organs or the nervous system.
(2) the havoc caused by Covid may have opened the door to latent pathogens.
(3) there may be an auto-immune reaction where the immune system is accidentally attacking its own body.
(4) gut bacteria is dysregulated.
(5) organ damage or other damage is triggering symptoms.
It’s possible that several of these theories are true, and that different subtypes of Long Covid have different combinations of these five explanations or even mechanisms that are not yet theorized.
What is not mentioned in the Vox piece or a similar New York Times piece is that a significant portion of patients may have Long Covid but no identifiable damage or disease process that explains their symptoms. It’s commonly known as “functional” or “medically unexplained” symptoms, and before the pandemic began, this category already accounted for as many as 10-30% of all emergency room and doctor visits. It’s very common, and it’s very frustrating for doctors and patients.
It is highly likely that a subtype of Long Covid is “functional,” meaning minimal or no damage, but horrible symptoms. As with functional syndromes like fibromyalgia (which has a similar constellation of symptoms like widespread pain, fatigue, insomnia, brain fog), the symptoms can be dramatically reduced.
Neuroplastic brain retraining (or a mind-body approach) can be very effective for functional somatic disorders, and there are evidence-based treatments available for them once they are identified. One of them, Emotional Awareness and Expression Therapy (EAET) has been shown to be effective in a randomized trial for patients with fibromyalgia, and was listed as a “best practice” by the Department of Health and Human Services on the strength of the data.
Also, it is possible that even for people who do have some structural damage, brain retraining may still be an effective method for reducing fear and unlearning symptoms.
It will take good research to sort that out.
NIH Study finds “Little To No Abnormalities” in LC Patients
A new NIH study finds that people with LC do not have damage that explains their symptoms. While some people will find this dispiriting, it can also be viewed as very good news. It means it’s possible to use brain retraining to reduce fear, regulate the nervous system, and unlearn fatigue and pain.
NPR interviewed one of the lead authors, Michael Sneller, MD, who conducted this study for the National Institutes of Health.
MICHAEL SNELLER, MD: So the thing that has struck me most now in a year and a half of seeing these patients and extensively testing them is that we are finding little to no abnormalities.
STEIN: He's tried every test he can think of.
SNELLER: Echocardiogram, pulmonary function tests, X-rays, brain MRIs, you name it, laboratory markers of organ dysfunction - not seeing any of that - and precious little evidence of immune activation looking just at the sort of the standard markers of inflammation. I'm running out of tests to do, basically.
STEIN: But Sneller hasn't ruled out anything and is still looking, including doing more detailed studies of the immune system, as well as psychological testing, because he agrees people are suffering real, long-lasting problems.
SNELLER: It's 100% real. These people have these symptoms - absolutely. The question is what's causing them. You know, just because you can't find - I mean, anxiety produces real symptoms. The symptoms are real. It's just they're not due to any damage we can pinpoint.
STEIN: But Akiko Iwasaki at Yale is convinced the immune system is playing a key role.
AKIKO IWASAKI, PHD: There is definitely something going on there. We need to know what that is. You know, we need to understand what's going on in each patient because the treatment option will be very different depending on what they actually have.
Our take on this scientific dispute: You could choose to decide Dr. Iwasaki is correct or Dr. Sneller and Dr. Donnino (who did the brain retraining at Harvard) are correct—they are smart researchers who fundamentally disagree—in fact they represent different worldviews of how healing works. Why pick one over the other?
We think the views of Dr. Sneller and Dr. Donnino are more hopeful for two reasons: 1. It means the body is healthy and not damaged—that is an extremely powerful message that can trigger the placebo effect and calm the nervous system. 2. There are proven treatments for functional syndromes, also known as mind-body or brain-generated illnesses. If you scroll up and listen to the LC recovery stories, you can get a sense of how brain retraining can lead to a full or substantial recovery through changing the brain-body connection. (Brain retraining can also lead to changes in biomarkers for stress and can alter the neuroanatomy of the brain.)
The view that Dr. Iwasaki represents is to wait for science to pinpoint the biomarkers of Long Covid and develop medications which will most likely take years to make it to market, if it ever happens. We think this is a more pessimistic view that is not in line with the latest neuroscience and advances in clinical medicine for functional syndromes, as depicted in our film. To learn more about brain-first treatments for Long Covid, check out our “how to unlearn pain” page.
Still hungry for more information? Believe it or not, there is additional resources and information on our spillover Long Covid page. Enjoy!
It is deeply meaningful for us to make this information available, and we hope you find it helpful. You can always reach Kent at tmhfilm@gmail.com with additions, thoughts, or queries.